Welcome to the America’s Criminologist Podcast for September 6, 2024. This is Dr Currie Myers with some interesting criminal justice news and events that have occurred in the United States recently. My Podcast is brought to you by the Howard Wagyu Ranch. Raised on a family ranch in Central Kansas, Howard Wagyu serves Wagyu beef with the highest quality and excellence. Just go to their Facebook Page and go to Howard Wagyu!
This week I was the guest host on the Lou Desmond Show on KMET in San Bernardino. Our guest this week Paul Mauro is a contributor for FOX News Media providing legal and criminal justice analysis across FOX News Channel and FOX Business Network programming. He joined the network in Mauro serves as a professor of law at John Jay College as well as a lawyer at DeMarco Law. Previously, he served as the Commanding Officer of the New York City Police Department’s Legal Bureau and the Executive Officer of the Intelligence Operations and Analysis Bureau. Throughout his career, Mauro has briefed members of the U.S. Congress, the National Counterterrorism Center, the Department of Justice, CIA, Department of Homeland Security, Interpol, Europol and other foreign and domestic entities. He also has a Substack that I highly recommend you subscribe to, called the Ops Desk. You can view that interview here.
I was also on the great Carl Jackson Show and I was his guest for the entire show. We discussed the rise in crime associated with illegal migrants, mass shootings and many other interesting areas. That show can be heard on radio, but it was also recorded for television. You can hear my interview with Carl here.
The Mental Health Crisis: Why We Enable Rather than Treat
As a society, we extend compassion to those battling physical illness in ways we rarely do for individuals grappling with mental illness. This disparity in treatment is glaring, given the widespread prevalence of mental health issues. Every year, approximately 25% of adults in developed countries experience significant mental health problems, yet the resources and responses to these challenges remain woefully inadequate. Mental disorders are often treated as acute, episodic ailments rather than the chronic illnesses they are. This outdated approach leaves millions of people without the proper care they need, leading to a worsening mental health crisis in the U.S.
Despite being a nation that values progress in medicine, we fail to deliver the same attention and care to mental illness as we do for physical diseases. Funding and awareness efforts for childhood and adult cancers are abundant and rightly celebrated, yet these efforts wane dramatically when it comes to mental health. The stigma surrounding mental illness, especially in children, stifles progress, leaving individuals suffering unnecessarily in silence. As an example, my research on California’s Proposition 47 was sold to the voters to spend less money on prisons and more money towards mental illness and drug abuse. What was the result? The quiet secret is that due to Prop 47, mandatory mental health and drug treatment options were removed from the judge's authority.
The Scale of the Crisis
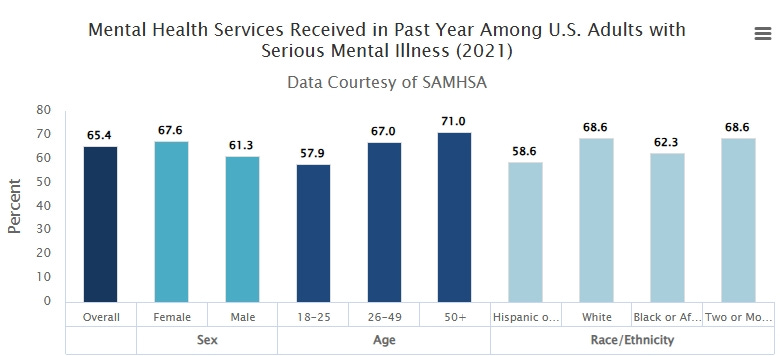
The numbers tell a distressing story. According to the National Alliance on Mental Illness (NAMI), 43.8 million adults in the United States experience mental illness each year. Among them, around 10 million people suffer from mental illness that severely interferes with major life activities such as work, school, and relationships. Yet, over half of these cases go untreated. This leaves individuals vulnerable and burdens families and communities left to deal with untreated mental health disorders.
Children are particularly vulnerable, with studies showing that half of all mental illnesses begin to show symptoms by age 14. Despite the early onset of these disorders, many go untreated due to the stigma associated with mental health care, especially when the patient is a child. Children may develop anxieties and phobias that serve as warning signs of more severe illnesses to come, yet parents and caregivers often hesitate to seek help, fearing societal judgment or misdiagnosis. The long-term consequences of ignoring early mental health challenges are profound. What could be treated early on becomes exacerbated by neglect, manifesting in chronic conditions that are far more difficult to manage in adulthood. The biggest underlining issue is that we have a significant reduction in quality of life. The three pillars of a successful society are faith, family, and formation. And all three pillars have suffered greatly over the last three decades. These pillars are included in the book I recently release called the “Advent of Feral Man.”
Failing the Chronically Ill
The current treatment model for mental illness is deeply flawed. Mental disorders, unlike many physical illnesses, are not episodic; they do not "go away" with temporary treatment or medication. They are chronic conditions that require long-term care and support, yet our healthcare system treats them as acute problems that only require attention when symptoms are severe or disruptive. This model leaves individuals in a perpetual cycle of crisis, without the consistent care they need to manage their illnesses effectively.
A 1994 study found that, by percentage of the population, there were 92% fewer hospitalized individuals with mental health issues than there were decades prior. While this decline might suggest progress on the surface, it is more likely a reflection of the disinvestment in mental health infrastructure. With fewer hospitals and long-term care facilities, patients are left to fend for themselves. This trend has continued, resulting in overburdened emergency rooms and jails that have become the de facto holding areas for individuals in crisis.
In many cases, individuals with severe mental illness end up homeless, incarcerated, or dead. And decriminalization of drug, especially synthetic drugs, has only exacerbated the problem. Data from a large nationally representative sample suggested that people with mental, personality, and substance use disorders were at increased risk for nonmedical use of prescription opioids It is a tragic cycle that reveals a systemic failure to address the needs of our most vulnerable populations. A 2014 NAMI report noted that approximately 26% of homeless adults staying in shelters live with serious mental illness. Additionally, about 24% of individuals in state prisons have a recent history of mental illness, a percentage that is higher for women. The prison system has become the new asylum, but without the resources or expertise needed to provide proper mental health care.
Stigma and Ignorance: Barriers to Treatment
A major barrier to effective mental health treatment is the persistent stigma surrounding it. Unlike cancer, heart disease, or diabetes, mental illness is often misunderstood as a sign of personal weakness or failure. The stigma creates shame and fear, discouraging people from seeking help. This is especially true for men, minorities, and older adults, who often feel additional cultural or societal pressure to "tough it out."
Stigma not only prevents individuals from accessing care, but it also affects public policy and funding decisions. Despite the prevalence of mental illness, funding for mental health services remains grossly inadequate. Public awareness campaigns for conditions such as breast cancer or heart disease inspire national action and generate billions in research funding. However, the same enthusiasm is absent when it comes to mental health, leaving vital services underfunded and understaffed.
The Cost of Inaction
The economic and social costs of untreated mental illness are staggering. Untreated mental health issues lead to lower productivity, higher rates of absenteeism, and an increased burden on social services and law enforcement. The cost to the U.S. economy due to serious mental illness is estimated to be more than $193 billion annually in lost earnings. This does not account for the costs of incarcerating mentally ill individuals, providing emergency care, or the devastating toll mental illness takes on families and communities.
Beyond the financial impact, the human cost is immeasurable. Every day, individuals with untreated mental illness are at risk of suicide, substance abuse, and violence—either directed at themselves or others. Mental illness can push people into isolation, destroying relationships and leading to despair. The tragic irony is that many of these outcomes are preventable with timely and appropriate care.
Mental Illness and Mass Shootings
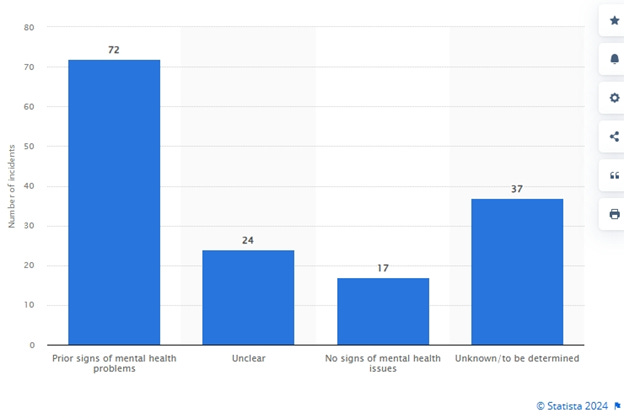
In 72 cases out of a total of 150 reported mass shootings in the United States since 1982, the shooter(s) displayed prior signs of mental health problems. In only 17 cases out of 150, there were no signs of mental health issues in the shooters.
And mass shootings have increase considerable over the last 8 years which coincided with the rise of mental illness. As of June 21, there was one mass shooting in the United States in 2024. This is compared to one mass shooting in 1982, one in 2000, and 12 mass shootings in 2022 and 2023.
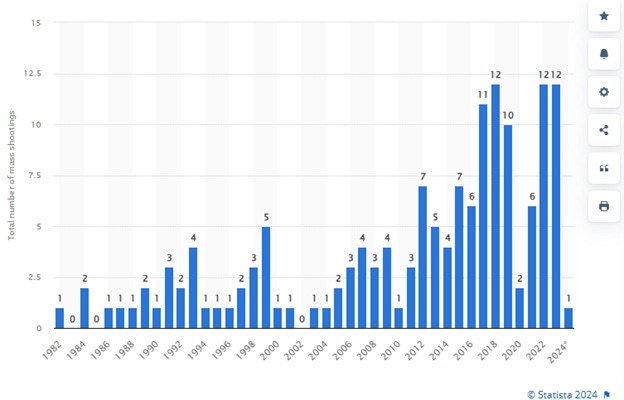
Note: Mass shootings, generally defined as incidents where four or more people are killed or injured by a firearm, excluding the shooter themselves.
A Call for Reform
Our current mental health strategy has become one of enabling rather than treating. Instead of investing in long-term care facilities, early intervention programs, and community-based services, we wait until individuals reach a crisis point before offering help. This reactive approach is not only costly, but it is also inhumane. We cannot continue to ignore the growing mental health crisis in this country.
One critical step towards reform is to implement a mental health care system that treats these disorders as chronic conditions requiring ongoing care, much like diabetes or hypertension. This could involve creating more mental health facilities, increasing the availability of inpatient beds, and expanding access to outpatient services.
Another step would be to mandate mental health care for individuals who are a danger to themselves or others. This should include mandated mental health screenings during the booking process for individuals entering the criminal justice system. By identifying and treating mental illness early, we could potentially reduce rates of incarceration and homelessness among those suffering from severe mental illness.
We are living in an age of significant social contagions, and those suffering from untreated mental illness are often among the most vulnerable to being lured into dangerous behaviors or ideologies. If we are serious about addressing this issue, we must acknowledge the full scope of the mental health crisis and commit to creating a system that provides care, not just in moments of crisis, but throughout an individual’s life.
The time for half-measures is over. We need a mental health care system that reflects the urgency and scale of the problem. And that’s my criminal justice memo for the week!
-My podcast also available on Spotify on America’s Criminologist with Dr. Currie Myers. And please join me on X @drcurriemyers
This is Dr Currie Myers, America’s Criminologist. To view my work please visit drcurriemyers.substack.com and please share and like our page! And please remember my friends at Howard Wagyu for some of the best beef in America. Howard Wagyu, Kansas homegrown Wagyu Beef so tender you can cut your steak with a fork!













Share this post